The post What Are the Most Common Pelvic Health Myths? appeared first on Hyivy.
]]>
When it comes to pelvic health for women and people with vaginas, there are a lot of myths out there. Hyivy Health was founded by Rachel Bartholomew who had no idea about how common, pervasive, and important pelvic health was until she started experiencing challenges of her own.
For today’s post we’re going to debunk what we see as the most common pelvic health myths out there, hopefully empowering you or someone you care about to move forward with more information on your pelvic health journey.
Myth #1: Kegels Are the Answer!
Kegel exercises aim to strengthen the pelvic floor muscles in order to support the uterus, bladder, small intestine, and rectum. Kegel exercises are typically performed by lifting, holding, and relaxing the pelvic floor muscles. Kegel exercisers (kegel devices) include insertable trainers, weights, and biofeedback devices.
But they are not for everyone and can for some people, kegels can cause serious damage.
Think of it this way, let’s say you’ve hurt your arm and now, you’re experiencing pain and can feel the muscles around the injury tensing up and making the pain worse. Would you then want to go to the gym and start lifting weights? – of course not!
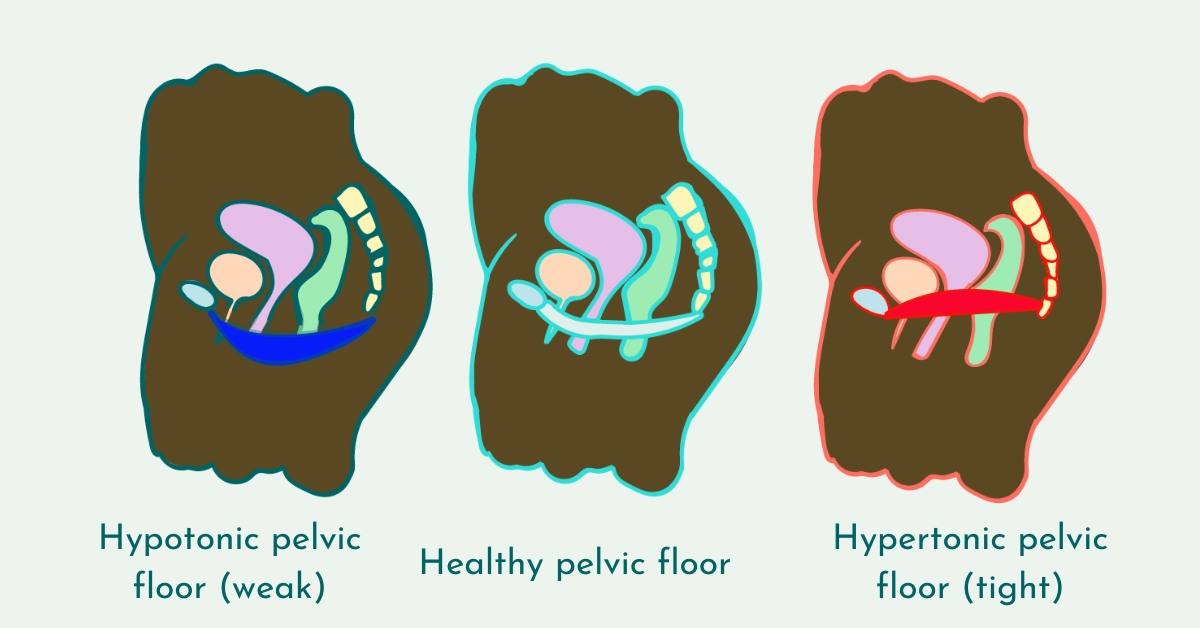
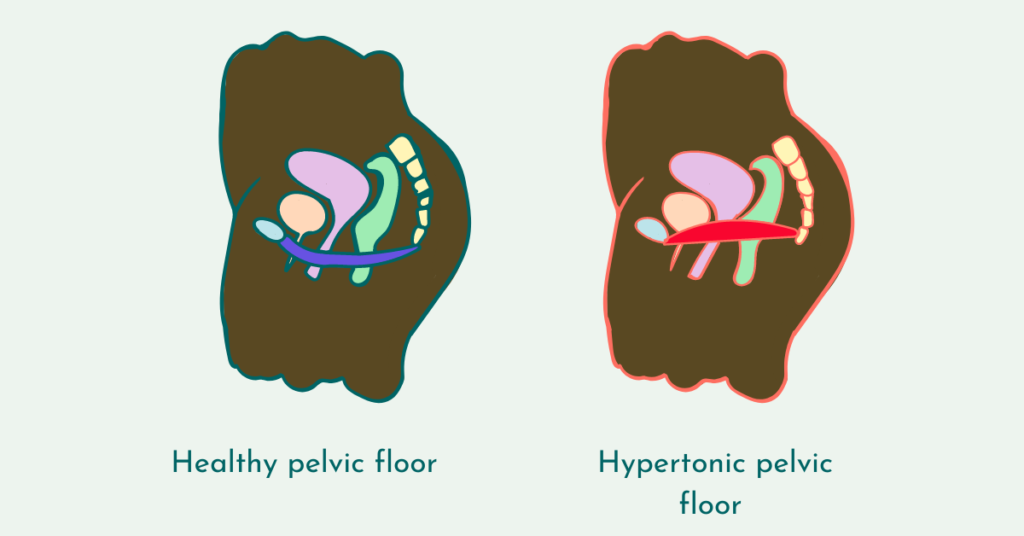
This serves as an analogy for folks who have a pelvic floor that’s too tight (hypertonic), and instead of working the muscles harder through kegels they need to relax these muscles to help relieve pain.
Currently, vaginal dilators are prescribed for this reason, and Hyivy is currently developing the first smart dilator that includes dilation without reinsertion, thermal therapy (hot and cold for those muscles), and biosensors to capture the first subjective and objective data on the pelvic floor.
 Myth #2:
Myth #2:
Pelvic Health Issues Only Affect Older People
Pelvic health issues affect 1 in 3 women across all ages and is not just an issue that affects people 65+. This myth might be so persistent because of the stigma and shame that surrounds pelvic health.
It’s important to know there are a range of pelvic health disorders and gynecological conditions that cause a wide range of pelvic floor issues including:
- Endometriosis
- Pelvic Cancers
- Vaginismus
- Vulvodynia
- Polycystic Ovary Syndrome (PCOS)
- Uterine fibroids
- Perimenopause and menopause
- Pregnancy and childbirth
- Dysmenorrhea (painful periods)
- Gender affirmation surgery
- Pelvic mesh complications
- Pelvic floor hypertoncity that ebbs and flows with your menstrual cycle and menopause
Myth #3: Sex Is Supposed to Be Painful
According to the American College of Obstetrics and Gynecologists (ACOG) painful sex is a very common problem with 3 out of 4 women and female identifying people experiencing painful sex at some point in their lives.
But that doesn’t mean you need to keep having painful sex. It’s important to see a healthcare professional to root out the underlying causes for your pain and potentially seek the help of a pelvic floor physiotherapist.
One thing to remember is that if you are experiencing painful sex, you are not alone. Everyone will take their own time to get to the amount of sexual activity they prefer. The most important thing is to listen to your body.
Myth #4: Pelvic Floor Physiotherapy is Only for People Who Have Given Birth
Although pelvic floor physiotherapy for pregnant and people who have given birth can be immensely helpful, these aren’t the only people who can benefit from seeing a Pelvic Floor Physiotherapist (PFPT).
PFPTs can help you with a wide range of pelvic health concerns. Some reasons you might want to seek out pelvic floor physiotherapy are:
- Pain in the (pelvis) pelvic, lower back, or genital region
- Urinary incontinence or frequency,
- Pelvic organ prolapse (POP)
- Pain with sex (dyspareunia) or when trying to insert a tampon
- Difficulty emptying the bladder or bowels.
What are some pelvic health myths you’ve come across on your pelvic health journey? Feel free to message us at hello[@]hyivy.com or DM us on Instagram at @ hyivyhealth so we can share across our social media channels.
—
Is there a blog topic you’d like us to cover? Reach out today to let us know.
Here at Hyivy Health we’re dedicated to helping women down there and everywhere. The purpose of this blog post is intended to offer resources and education about pelvic health and is not intended to serve as medical advice. This information provided above is not a substitute for the treatment, advice, or opinion of a medical professional. Always consult with a certified health professional before starting any treatments.
The post What Are the Most Common Pelvic Health Myths? appeared first on Hyivy.
]]>The post What is Chronic Pelvic Pain? appeared first on Hyivy.
]]>What is Chronic Pelvic Pain?
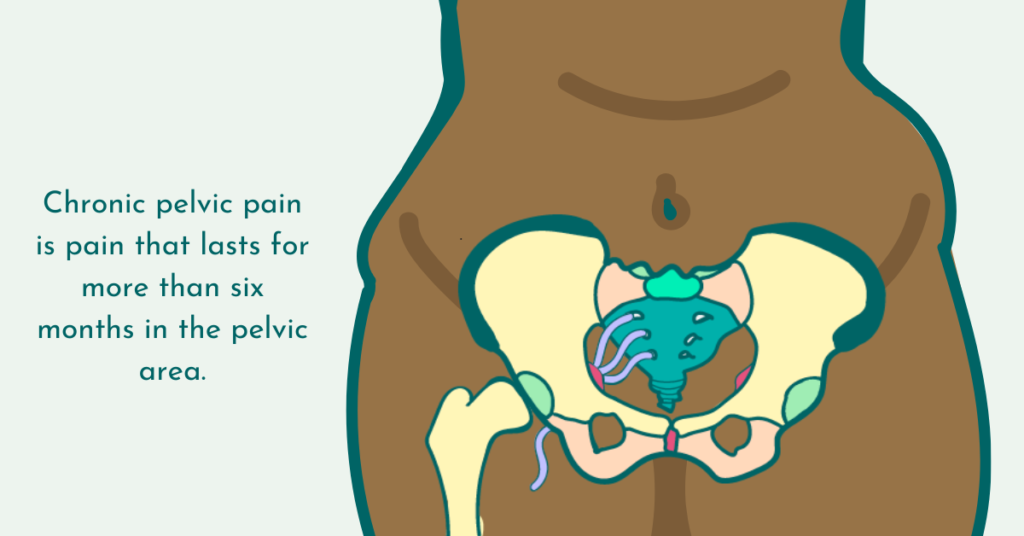
Chronic pelvic pain is pain that lasts for more than six months in the pelvic area.
This pain can be experienced constantly, on a regular cycle, or only at certain times. For example, you might only experience this pain when menstruating, emptying your bladder, during or after sexual intercourse, or from sitting or standing for long periods of time.
Although chronic pelvic pain is very common, with as many as 25% of women experiencing this at some point in their lives, there’s been a lack of research into the exact mechanisms of chronic pelvic pain.
What Does Chronic Pelvic Pain Feel Like?
Chronic pelvic pain can be felt in different areas of your pelvis, not just one spot every time. Chronic pelvic pain can be mild to moderate or be so intense they might cause you to miss work or prevent you from living the way you prefer.
Chronic pelvic pain can be described in several ways including:
- Pressure or heaviness in the pelvis
- Dull aching
- Serious and steady
- Pain that comes and goes
Because many of the conditions leading to chronic pelvic pain cause your pelvic floor to become too tight or tense up (hypertonic) and the pelvic floor acts as a hammock that supports your organs including your bowel, bladder, and uterus you may also experience symptoms like:
- An urgent or frequent need to urinate
- Abdominal bloating
- Gastrointestinal problems like upset stomach or IBS
- Constipation
What Causes Chronic Pelvic Pain?
There are a range of conditions that can cause chronic pelvic pain and it’s important that you see a healthcare provider as soon as possible when you start experiencing symptoms.
Some conditions that cause chronic pelvic pain include but are not limited to:
- Endometriosis
- Side effects from radiation in your pelvic area (radiation induced vaginal stenosis)
- Uterine fibroids
- Pelvic inflammatory disease
- Pelvic floor injury caused by an accident, pregnancy, or childbirth
- Interstitial cystitis, also known as painful bladder disease
- Dysmenorrhea (painful periods)
How is Chronic Pelvic Pain Treated?
The first step to treating chronic pelvic pain is seeing a healthcare professional who will take a medical history, ask you about your daily life, and conduct a pelvic exam.
Depending on your diagnosis the underlying condition may be treated with medication for infection, hormonal birth control for issues with menstruation, or potentially surgery.
For many people with chronic pelvic pain, managing the pain and severity is achieved through:
- Pelvic Floor Physiotherapy – Pelvic floor physiotherapists (or PFPTs) work to help you rehabilitate your pelvic floor muscles. They are specially trained to conduct internal and external assessments and treatments for your pelvic floor. Learn more about what to expect from your first pelvic floor physio appointment. [link to blog]
- Vaginal dilators – Vaginal dilators (inserts) are plastic or silicone rods or cylinders with a rounded tip. They are meant to open (dilate) and stretch the tissues of the vagina.
- Cognitive behavioral therapy or sex therapy – this does not mean that your pain is not real or “all in your head” but rather, a licensed professional may help to support you through your treatment plan
Hyivy Health is currently working with researchers across the world to help grow our knowledge base of how chronic pelvic pain works and how to better treat it. We’re currently developing a smart vaginal dilator with multi-therapy capabilities which will be the first ever to collect both subjective and objective data on the pelvic floor which will be shared with clinicians through our clinician software.
If you or someone you know is interested in participating in focus groups and potential product testing, reach out today.
—
Is there a blog topic you’d like us to cover? Reach out today to let us know.
Here at Hyivy Health we’re dedicated to helping women down there and everywhere. The purpose of this blog post is intended to offer resources and education about pelvic health and is not intended to serve as medical advice. This information provided above is not a substitute for the treatment, advice, or opinion of a medical professional. Always consult with a certified health professional before starting any treatments.
The post What is Chronic Pelvic Pain? appeared first on Hyivy.
]]>
What is Painful Sex?
Painful sex, or dyspareunia (dis-puh-ROO-nee-uh) is pain in your genitals or pelvic area occurring before, during, or after sexual intercourse.
Sexual intercourse comes in a wide and unique variety of forms and may mean different things to different people. This can include genital-to-genital, mouth-to-genital, and toy-to-genital contact as well as penetration and stimulation of the anus.
Although painful sex can affect all kinds of folks, today’s post will be focusing on dyspareunia experienced by people with vulvas and vaginas that involves the act of penetration by a penis, fingers, or toys.
Is Painful Sex Normal?
According to the American College of Obstetrics and Gynecologists (ACOG) painful sex is a very common problem with 3 out of 4 women and female identifying people experiencing painful sex at some point in their lives.
Some people may experience painful sex for a short period of time, while for others this can be a lifelong problem that can severely impact relationships, quality of life, and mental health.
Although painful sex is common, it’s not normal.
There are multiple reasons why you might be experiencing pain during sex. It’s important you always speak to a medical professional to help you identify the reason, or multiple reasons, why you’re experiencing pain as the first step towards pain-free sex.
What Does Painful Sex Feel Like?
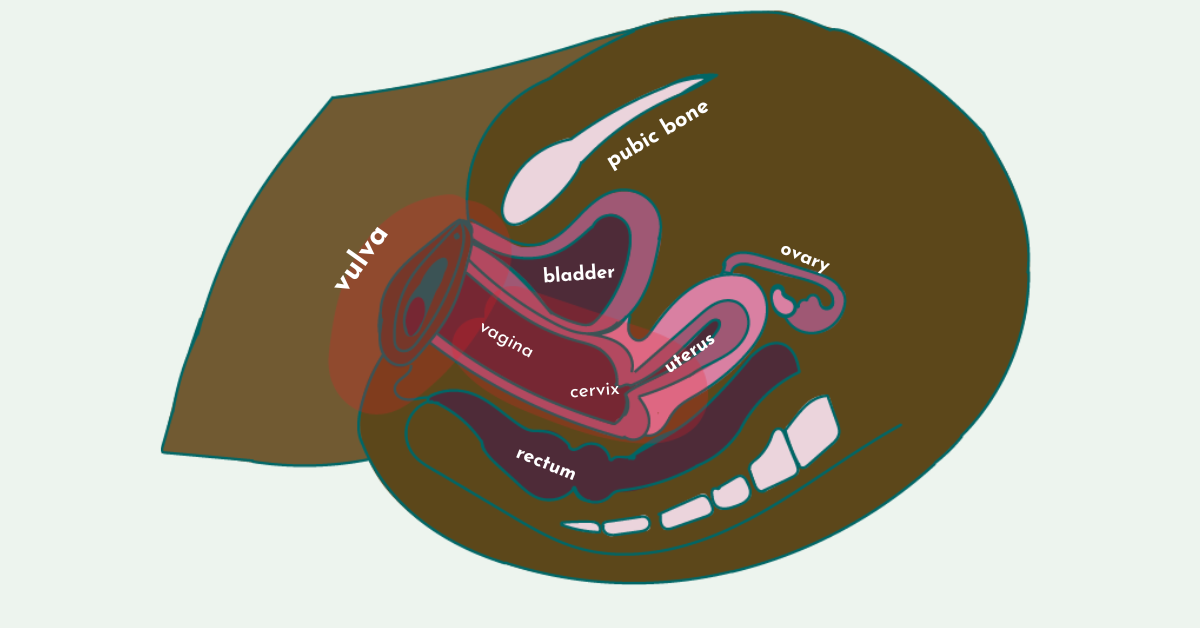
If you’re experiencing painful sex, you may feel pain in your vulva, the area surrounding your vagina called your vestibule, within your vagina, and in your perinium.
Dyspareunia can be experienced as:
- Entry Pain (intraorbinal or superficial) is pain you feel at the entrance of the vagina with penetration
- Deep pain (collision) is pain you feel with deep penetration in your cervix or lower abdomen, this can worsen with different positions
Painful sex is also sometimes categorized as primary, secondary, complete, or situational:
- Primary pain is pain that you’ve always experienced since becoming sexually active
- Secondary pain is pain that develops after having a time of experiencing pain free sex
- Complete pain is when you experience pain every time you have sex or with any insertion including a finger, tampon, or toy
- Situational pain is when the pain only happens in certain situations or positions
Some sensations of painful sex include:
- Stabbing or sharp pain with penetration
- Deep pain with thrusting
- Aching or throbbing after intercourse
- A feel of burning
- Pelvic cramps that feels like menstrual cramping
- A feeling a muscle spasms or tightness
What Causes Painful Sex?
Some causes for painful sex include:
- Vulvodynia
- Vaginismus
- Vaginal atrophy or dryness caused by medication, menopause or other hormonal issues
- Radiation induced vaginal atrophy
- Vaginal infections like yeast infections
- Endometriosis
- Uterine fibroids
- Pelvic inflammatory disease
- Sexually transmitted infections (STIs)
- Intercourse too soon after childbirth
- Injury to the vulva or vagina including tears or cuts
- Skin allergy or irritation
How Is Painful Sex Treated?
Treatment will depend on your diagnosis and what your underlying issues are.
Some common treatments include:
- Medications to treat infections and allergies
- Estrogen creams or tablets for vaginal dryness or atrophy caused by decreased hormone levels
- Vaginal dilators to help to gradually stretch and relax the pelvic floor muscles
- Pelvic floor physiotherapy
- Talk therapy with a certified professional
One thing to remember is that if you are experiencing painful sex, you are not alone. Everyone will take their own time to get to the amount of sexual activity they prefer. The most important thing is to listen to your body.
————
Is there a blog topic you’d like us to cover? Reach out today to let us know.
Here at Hyivy Health, we’re dedicated to helping you down there and everywhere. The purpose of this blog post is to offer resources and education about pelvic health and is not intended to serve as medical advice. The information provided above is not a substitute for the treatment, advice, or opinion of a medical professional. Always consult with a certified health professional before starting any treatments.
The post Is Painful Sex Normal? appeared first on Hyivy.
]]>
What is Endometriosis?
Endometriosis is a chronic condition in which tissue similar to endometrial tissue grows outside of the uterus (womb), causing scar tissue and/or adhesions in the pelvic region including the ovaries and fallopian tubes.
Over 70% of people with chronic pelvic pain have endometriosis and it is one of the most common pelvic diseases.
Even though this tissue is outside of where it belongs, it continues to behave as it would if it was in your uterus, so with your menstrual cycle this endometrial tissue thickens, breaks down, and bleeds.
Since this blood has no way to exit your body, it becomes trapped. When endometriosis affects your ovaries, cysts called endometriomas may form. In your pelvic area, the surrounding tissue becomes irritated, eventually developing scar tissue and bands of fibrous tissue that can cause areas of your pelvic and organs to stick together.
Recordings and research go as far back as the 1700s with descriptions of “chocolate cysts” in the female reproductive system, and in the 1930s saw the discovery of the rare cases when endometriosis is found in other parts of the body including the lungs, bowels, colon, rectum, bladder, lymph nodes, and cervix.
Despite the fact that we’ve known about endometriosis for centuries, it is still a commonly misdiagnosed condition with many people waiting up to 10 years for their official diagnosis.
What are the Signs and Symptoms of Endometriosis?
One of the most common symptoms of endometriosis is chronic pelvic pain. Although it’s normal to have some cramping and discomfort during your period, pain that causes you to miss out on work, school, or social activities isn’t normal.
In addition to chronic pelvic pain, signs and symptoms of endometriosis include:
- Mild to severe pain in your back, abdomen, and pelvis during menstrual periods
- Pain with sexual intercourse (dyspareunia)
- Painful bowel movements and/or urination
- Heavy bleeding during menstrual periods
- Nausea, fatigue, depression, and anxiety
- Fertility complications such as increased difficulty in getting pregnant
How is Endometriosis Diagnosed?
The current standard of care when it comes to an endometriosis diagnosis is a laparoscopic surgery (also known as keyhole surgery) where a small incision is made your abdomen where a small telescope is inserted so that your doctor can look for adhesions and then potentially remove them.
Some people with endometriosis don’t have any symptoms at all and are only diagnosed if abnormal tissue is discovered during a routine procedure or surgery.
Odds are that you or someone you know has or suspects they have endometriosis, considering that 1 in 10 women are affected by this disease.
How is Endometriosis Treated?
Treatment for endometriosis is a personalized plan that includes medications and surgery. Currently there is no cure for endometriosis. Only a certified medical professional can figure out the right course of action for you.
When it comes to managing and treating chronic pelvic pain, a Pelvic Floor Physiotherapist (PFPT) can provide hands on treatment to help manage your pain and reduce pelvic floor tightness (hypertonicity) which can help with your pelvic pain, back pain, painful urination, and painful bowel movements.
The tightening of these muscles can also lead to painful intercourse, which a PFPT has a range of in-clinic and at-home techniques including vaginal dilators to massage, relax, and breakdown scar tissue and relieve pain.
Where Can I Get More Information About Endometriosis?
If you are currently dealing with, or suspect you have endometriosis, you are not alone. There are a variety of organizations you can join or check out to get more information, share your story, connect with others, and get support:
- Nancy’s Nook
- EndoBlack
- The Endometriosis Network Canada
- Endometriosis Association
- Endometriosis.org
- Endometriosis Foundation of America
————
Is there a blog topic you’d like us to cover? Reach out today to let us know.
Here at Hyivy Health, we’re dedicated to helping you down there and everywhere. The purpose of this blog post is to offer resources and education about pelvic health and is not intended to serve as medical advice. The information provided above is not a substitute for the treatment, advice, or opinion of a medical professional. Always consult with a certified health professional before starting any treatments.
The post What is Endometriosis? appeared first on Hyivy.
]]>The post What Should I Expect for my First Pelvic Floor Physiotherapy Appointment? appeared first on Hyivy.
]]>Pelvic floor physiotherapy is available to all kinds of folks for a wide range of reasons. For the purposes of today’s blog post we’ll be focusing on women or people with a uterus, vagina, vulva, and vaginal canal.
We’re also joined by Keri Martin Vrbanac Registered Physiotherapist, Pelvic Floor Physiotherapist, and Clinic Owner at A Body in Motion Rehabilitation Clinic to help answer some more specific questions about PFPTs and their work.
Symptoms that might cause you to seek out the pelvic floor physiotherapy are pain in the (pelvis) pelvic, lower back, or genital region, urinary incontinence or frequency, pelvic organ prolapse (POP), pain with sex (dyspareunia) or when trying to insert a tampon, or difficulty emptying the bladder or bowels.
Pelvic floor muscles are like any other in the body, and can become weak or too tight, or a combination of the two. For more in-depth information check out our recent post on the difference between a hypertonic and hypotonic pelvic floor.
What is a Pelvic Floor Physiotherapist?
Pelvic floor physiotherapists (or PFPTs) work to help you rehabilitate your pelvic floor muscles. They are specially trained to conduct internal and external assessments and treatments for your pelvic floor.
One thing Keri made sure to point out is that a PFPT’s job is to make sure that you always feel comfortable with your care.
“What I always say to my patients, I will be telling you every single thing that I am going to do before I do it. If at any time you are uncomfortable with, you just let me know and we will stop. You are 100% in control of your consent, and if you ever need to withdraw your consent, that’s totally within your right,” says Keri.
What Should I Expect from My First Appointment?
Although pelvic health issues are very common, we know how difficult it might feel to finally make that appointment to see a PFPT, so the first thing is to congratulate yourself for taking the time to care for yourself and taking time out for you!
When it comes to your first appointment, the trained administration staff will book your appointment and answer any admin questions you might have and your PFPT will work to understand a holistic picture of your health in order to create an individual plan of treatment for you.
As Keri likes to put it, “What I always say to patients, is I’m going to treat you like an onion, we’re going to start on the outside and we’re going to peel away the layers. As a Pelvic Floor PT I am concerned with your body from head to toe, I don’t just focus on the pelvis.”
When you meet your PFPT the first part of the session will be a conversation, they’ll ask you questions about your history with pelvic health to get to know more about what’s brought you there and what your goals are.
Many of us with pelvic health issues have been experiencing these problems for a long time, even decades, so don’t be shy about taking the time to share your entire story. Keri likes to start with the question, “tell me your story.”
What is an Internal and an External Pelvic Floor Assessment?
Your pelvic floor is made up of the same elements as the rest of your body including joints ligaments, connective tissue, and tendons. An internal and external exam of these elements are a way to get a full picture of your health. Depending on your condition, your first appointment may or may not have an internal exam, “We are able to see and feel externally but internal assessments provide a clearer picture”, says Kerri.
An external exam can include your PFPT examining your flexibility by asking you to touch your toes, checking your reflexes or asking whether you’ve experienced numbness or tingling.
An internal exam includes your PFPT leaving the room so you can remove the clothing from the lower half of your body and cover up in a sheet for comfort.
The great news: it’s not like a PAP smear at the gynecologist’s office, so no scooting down or cold metal stirrups. You’ll be positioned on your back with your knees bent.
When the PFPT returns they will articulate each step they’re taking which can include observation, palpation, and special tests. They may check your vulva and labia for any discoloration or issues.
Many PFPTs use their fingers inserted in the vagina and rectum and may ask you to “bear down” or squeeze to get a sense of where your organs are positioned. Some PFPTs will use a biofeedback device to assess pelvic floor function.
An internal exam should never be painful. If you are experiencing discomfort, tell our PFPT and they will stop right away.
What Should I Wear to My Pelvic Floor Physiotherapy Appointment? (And other questions)
Short answer: something comfortable! You’ll either be sitting and talking or laying on your side or back, so whatever makes you feel the most like you.
What about shaving or waxing, you might ask?
“I don’t notice if you’ve shaved, I don’t care. I don’t care if your legs are hairy, I don’t care if you haven’t had time to get a pedicure. I want you to come to me as your best self and be comfortable with what I’m doing and that’s it,” says Keri.
Note: it’s always a good idea to check with your local COVID-19 mask requirements ahead of time so you know what’s appropriate for your appointment.
—
Is there a blog topic you’d like us to cover? Reach out today to let us know.
Here at Hyivy Health we’re dedicated to helping women down there and everywhere. The purpose of this blog post is intended to offer resources and education about pelvic health and is not intended to serve as medical advice. This information provided above is not a substitute for the treatment, advice, or opinion of a medical professional. Always consult with a certified health professional before starting any treatments.
The post What Should I Expect for my First Pelvic Floor Physiotherapy Appointment? appeared first on Hyivy.
]]>There are many reasons why you might be experiencing issues with your pelvic floor. You might have symptoms that are mild and annoying, or you might have gotten to the point where your symptoms are interfering with your daily life.
In this post, we’re going to outline what the pelvic floor is, the differences between a hypertonic and hypotonic pelvic floor, and why it’s important to get appropriate treatment for both conditions.
WHAT IS THE PELVIC FLOOR?
Your pelvic floor muscles are a group of muscles that stretch from the tailbone to the pubic bone at the front and between the sitz bones from one side to the other. They act as a hammock, providing support for your pelvic organs.
One way to feel your pelvic floor is to imagine picking up a cherry with your vagina (if you have one) – you’d be using your pelvic floor muscles to do that!
WHAT IS A HYPERTONIC PELVIC FLOOR?
A hypertonic pelvic floor occurs when your pelvic muscles are too tight or tense and can’t relax. Hypertonic pelvic floor is also known as pelvic floor tightness or hypertonicity. Signs and symptoms of a hypertonic floor include:
- urge or overflow urinary incontinence – impacting frequency (having to pee often), urgency (a sudden, strong need to pee), or hesitancy (having trouble starting the stream or keeping it going)
- painful urination
- incomplete emptying of the bladder
- constipation or straining during bowel movements
- pain during or after bowel movements
- unexplained pain in your low back, pelvic region, hips, genital area, or rectum
- pain during or after sexual intercourse (dyspareunia), sexual stimulation, orgasms, or vaginal penetration
- uncoordinated muscle contractions causing the pelvic floor muscles to spasm
There isn’t one single reason or cause for a hypertonic pelvic floor. However, some contributing activities or conditions that have been linked to pelvic floor hypertonicity include:
- repeatedly holding your urine or feces for long periods
- tensing the core muscles in workouts
- sexual trauma
- high levels of stress or anxiety that might cause you to frequently tense your pelvic floor
- chronic pain caused by endometriosis or irritable bowel syndrome (IBS) that can cause you to tense your pelvic floor muscles
- conditions like interstitial cystitis, pudendal neuralgia, or vulvodynia
- birth trauma, including scarring or one-sided pelvic floor tears
- cancer treatments, such as internal and external radiation
- surgeries to the pelvic area
It’s very important to see a specially trained doctor or pelvic floor therapist if you are experiencing any of these symptoms so that they can identify the root cause of your hypertonic pelvic floor. Once diagnosed, a pelvic floor therapist may offer you:
- suggestions for pelvic muscle relaxation, including breathing techniques
- advice on bladder and bowel habits (for example, no straining)
- pelvic floor and abdominal massage techniques
- scar tissue massage techniques
- pelvic and hip stretches
WHAT IS A HYPOTONIC PELVIC FLOOR?
A hypotonic pelvic floor occurs when your pelvic muscles are too weak to function how they’re supposed to and aren’t able to properly support the pelvic floor organs.
Hypotonic pelvic floor is also known as pelvic floor weakness or hypotonicity. Signs and symptoms of a hypotonic pelvic floor include:
- stress urinary or fecal incontinence (leaking of urine or feces)
- pressure in your pelvic area that can lead to pain
- pelvic organ prolapse (when one or more organs drop against the vagina)
- decreased sensation (feeling less) during sexual intercourse
There isn’t one single reason or cause for a hypotonic pelvic floor. However, some contributing activities or conditions that have been linked to pelvic floor hypotonicity include:
- trauma to the pelvic floor (such as a car accident)
- pregnancy and giving birth
- chronic constipation
- interstitial cystitis , which can cause pain in the pelvic floor muscles and loss of muscle strength
- menopause and aging
Once diagnosed, a pelvic floor therapist may offer you:
- specialized exercises to help to strengthen the pelvic floor (kegels)
- use of a biofeedback device
WHY IS IT IMPORTANT TO KNOW THE DIFFERENCE?
It’s important to know the difference between hypertonic and hypotonic pelvic floor because they’re both treated very differently.
Many people think that when they start to experience pelvic pain, urinary incontinence, or leaking that all they need to do is start kegel exercises or buy a kegel trainer to tighten their pelvic floor muscles. However, if you have a hypertonic pelvic floor, these exercises can make the problem worse. Ignoring your symptoms or just waiting to see if they go away can also lead to worsening symptoms.
When in doubt, remember to put your health and wellness first by seeing a certified health professional who’s trained specifically to diagnose and treat the pelvic floor.
Hopefully after you read this article you will feel more empowered to understand the difference between the hypertonic and hypotonic pelvic floor and understand why it’s so important for you to know the difference.
————
Is there a blog topic you’d like us to cover? Reach out today to let us know.
Here at Hyivy Health, we’re dedicated to helping you down there and everywhere. The purpose of this blog post is to offer resources and education about pelvic health and is not intended to serve as medical advice. The information provided above is not a substitute for the treatment, advice, or opinion of a medical professional. Always consult with a certified health professional before starting any treatments.
The post What’s the Difference Between a Hypertonic and Hypotonic Pelvic Floor? appeared first on Hyivy.
]]>What is the Pelvic Floor?
The pelvic floor is a group of muscles that stretch from the tailbone (also known as the coccyx) to the pubic bone at the front and between the sitz bones from one side to the other.
Think of your pelvic floor as a hammock just under your core, making sure everything stays in place. The 36 muscles that make up your pelvic floor all work to support pelvic organs like the vagina, cervix, uterus, bladder, urethra, uterus, prostate, and rectum.
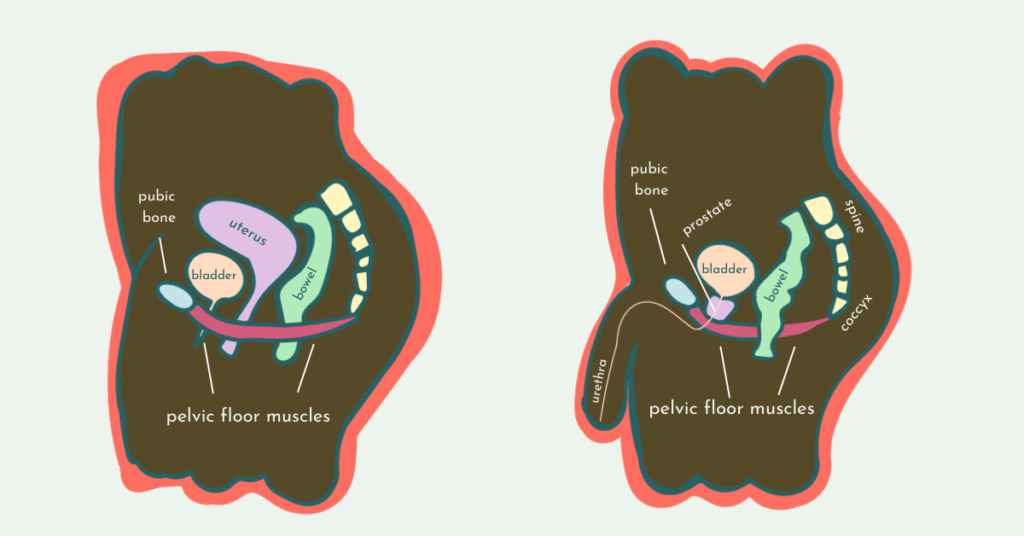
The pelvic floor muscles are like a hammock supporting all of your pelvic organs
What does the Pelvic Floor do?
The pelvic floor muscles provide the main support for the pelvic organs, but serve multiple other functions, including:
- Urinary continence
- Fecal continence
- Sexual intercourse
- Orgasms and erections
- Vaginal delivery during childbirth
The pelvic floor isn’t an isolated group of muscles that handle going to the bathroom and reproduction and sexual function. Pelvic floor muscles also provide stability for your core and involve complex coordination between somatic and autonomic motor nervous systems. Somatic motor functions are voluntary actions like standing or sitting, and autonomic motor functions are involuntary like breathing or blinking.
For example, you don’t have to think about the pelvic floor muscles that are working together to keep your pelvic organs like your bladder or uterus in place. But now think about stopping urine midstream when you’re peeing – those are some of your pelvic muscles at work.
Now imagine you’re trying to pick up a cherry from the floor with your pelvic floor muscles. You’re going to have to voluntarily squeeze some of them, right? (You’re also probably never going to look at a cherry the same way again!)
Hyivy Health’s 5 Pelvic Floor Vital Signs
The purpose of this list is to give you a sense of the various ways your pelvic floor can be thought about, felt, monitored, and cared for:
1. Sensation
The pelvic floor has a wide range of physical reactions and sensations, including sexual response and orgasm. The symptoms to look out for when you may need to consult a clinician are: chronic pain (pain that continues for more than three months), loss of libido, inability to achieve arousal, or discomfort.
2. Lubrication
The level of moisture in the pelvic floor is subject to hormonal changes and there is a unique level of discharge and lubrication for every individual.
The symptoms to look out for when you may need to consult a clinician are: irregular discharge including watery consistency, abnormal color, or increased frequency, and chronic vaginal dryness (dryness that continues for more than three months).
3. Incontinence
The pelvic floor is responsible for both urinary and bowel control.
The symptoms to look out for when you may need to consult a clinician are: pain with urination, increase in urinary frequency (overactive bladder), or loss of urinary or bowel control.
4. Health of tissues
Usually, we don’t notice the health of tissues until something is wrong.
The symptoms to look out for when you may need to consult a clinician are: stenosis (narrowing and shortening of the vagina), sores and rashes, thinning of the skin in the vagina or on the vulva, redness, irritation, itching, bleeding, or atrophy.
5. Muscle control and response
The inability to correctly relax and coordinate your pelvic floor muscles is called pelvic floor dysfunction.
The symptoms to look out for when you may need to consult a clinician are: pelvic muscle weakness (hypotonic) and overactive pelvic muscles (hypertonic). For more in-depth details on these symptoms, check out our blog post on the difference between a hypertonic and hypotonic pelvic floor.
—
Is there a blog topic you’d like us to cover? Reach out today to let us know.
Here at Hyivy Health, we’re dedicated to helping you down there and everywhere. The purpose of this blog post is to offer resources and education about pelvic health and is not intended to serve as medical advice. The information provided above is not a substitute for the treatment, advice, or opinion of a medical professional. Always consult with a certified health professional before starting any treatments.
The post What Do I Need to Know About the Pelvic Floor? appeared first on Hyivy.
]]>